Knee Replacements
What Exactly Is A Knee Replacement?
A knee replacement, otherwise known as a knee arthroplasty, is a surgical procedure to replace either part of or the whole of the knee joint. Performed by an Orthopaedic Surgeon, these surgeries hospital stay of a week or so.
How Common Are Knee Replacement Surgeries?
Knee replacements is a common orthopaedic procedure in Australian hospitals. In Australia, 62,800 knee replacements were performed in 2020-21, compared to 38,800 hip replacements (AIHW, 2023).
What Are The Reasons For A Knee Replacement?
There are multiple reasons for needing a replacement… whether it’s due to degenerative changes, traumatic injuries or as a measure to help people manage better with less pain in their knee. A common group we see though are older adults who are having increasing issues with Osteoarthritis (OA) in their knees.
“In Australia, 1 in 5 adults over the age of 45 have Osteoarthritis”
Knee Osteoarthritis can be divided into two categories
Primary Knee OA which refers to degenerative changes in the articular cartilage which can’t be attributed to a particular cause though changes become more common as we progress through the lifespan
Secondary Knee OA refers to degenerative changes that can be attributed to a particular cause. These causes my include obesity, prior traumatic injury, immobilisation, joint instability / hypermobility, and Vitamin D deficiency
It is important to keep in mind that any changes in your knees don’t necessarily lead to a joint replacement. In fact the Royal Australian College of GP’s Guideline for managing Knee OA recommends referral to a surgeon ONLY when conservative options have failed for end-stage OA.
Functional Knee Anatomy
The knee is the largest joint in the body. Not just one joint, but consisting of three seperate joints!
The bones involved in making up the knee are;
Tibia or your shin bone and the top section provides a platform for your thigh to rest on.
Patella or the kneecap acts as a fulcrum to transfer the force of your thigh muscles on to the Tibia.
Femur or the thigh bone and is also the largest long bone in your body. The bottom of this bone rests on top of the Tibia.
Fibula which runs down the outside of your Tibia
Yes, There Are Three Knee Joints!
Tibiofemoral (Tibia & Femur) Joint: This joint is classified as a ‘Modified Hinge’ joint, and its primary motions are flexion / extension and external rotation of the Tibia.
Patellofemoral (Patella & Femur) Joint: It is classified as a “Saddle” joint, and the primary motions are gliding up, down, and side to side relative to the tibiofemoral joint.
Superior Tibiofibular (Tibia & Femur) Joint: This is the joint located at the top of the Tibia and Fibula and it is classified as a 'Plane” joint. The primary motions here are to allow the two bones to move forwards / backwards, up / down, and rotate in relation to each other.
To make things more confusing, the bones and joints are grouped in to 3 compartments.
Lateral Compartment (Outside Part Of The Knee)
Consisting of the lateral end of the Femur and the lateral end of the top of the Tibia.
Medial Compartment (Inside Part Of The Knee)
Consisting of the medial end of the Femur & the medial top of the Tibia.
Patellofemoral Compartment (Front Of The Knee)
Consisting of the Patella and the end of the Femur.
What Are The Treatment Options For Knee OA?
Historically knee surgeries such as a total knee replacement or an arthroscope were one of the first lines of treatment in knee OA. As time has gone on however, the focus on surgery has diminished, instead shifting towards education, exercise & pain relief as needed.
First Treatments
Education, Exercise & Weight advice are indicated for all people experiencing knee pain from OA
Second Treatments
This is the introduction of strategies to help you with your symptoms. This might be medicine, bracing or passive therapies but is only required in some cases
Third Or Last Treatment Options
This includes surgeries but are only indicated in severe cases and should only be utilised when the other treatments are no-longer helpful
Conservative Management
In individuals with Knee OA, conservative management with a Physiotherapist is typically the first line treatment. The aim of this is to address the restrictions in knee range of motion, pain, strength and functional limitations. The symptom in particular conservative management aims to address is knee pain, as the associated reduction in functional ability strongly relates to future disability and dependency. As a result, early treatment of the associated pain related functional decline is vital for treating OA & other forms of knee pain (Farrokhi et al; 2016).
Strength training
Strength training is one of the core components for conservative management of knee OA. Exercises generally focus on lower limb strengthening, but can include upper limb exercises as well.
According to Vincent et al; (2012), the basic components of a lower limb strengthening program for knee OA include;
Squatting type exercises
Knee Extension
Knee Flexion
Other common exercises that are commonly prescribed in the conservative management of knee OA target hip abduction/ adduction, and ankle strength. The reasoning behind this is addressing any potential contributing factors to altered kinematics of the knee (Vincent et al; 2012).
GLA:D Protocol
One of the most popular lower limb strengthening strategies utilised by physiotherapists is the Good Living with Osteoarthritis in Denmark, or GLA:D, program. It has been demonstrated to improve pain intensity and quality of life for people with osteoarthritis (Skou et al; 2017). The GLA:D program is a structured exercise & education program, with guidelines around exercise prescription, dosage, and education surrounding the prognosis of OA.
Education around the pathology of osteoarthritis, prognosis, and exercise almost always form a major part of conservative management. This forms a part of the GLA:D protocol, with 8 weeks of education a core component of it.
Knee Replacement Surgery - When All Else Fails
If all conservative management strategies for knee OA fail to improve the quality of life for the individual to an adequate level, then surgical interventions is the next port of call.
Osteoarthritis is the most common condition leading to both hip and knee replacements, with this trend increasing by on average 2.6% per year between 2010-11 & 2020-21 (AIHW, 2023).
Knee replacement surgery can offer good outcomes for patients who require these surgeries, but it is important to discuss with your surgeon the risks & benefits of each procedure to ensure your expectations are in line with each other.
Main types of knee replacement
There are two main types of knee replacements. The first one is a Partial knee replacement, otherwise known as a Unicompartmental knee placement. The second one is a Total knee replacement, also known as a total knee arthroplasty.
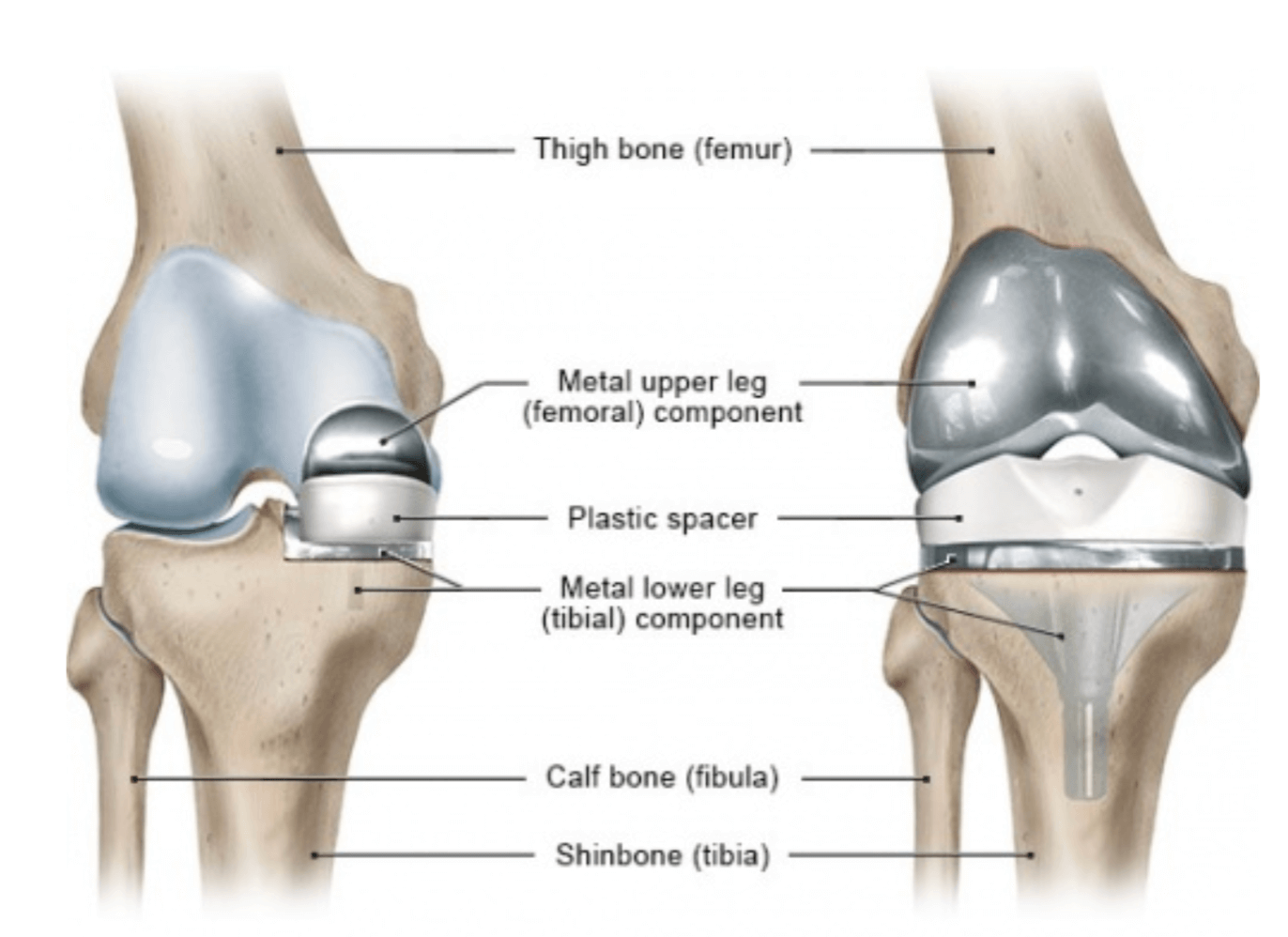
In a Partial knee replacement (UKR) only one portion of the thigh bone (femur) is replaced, along with the corresponding portion of the shin bone (tibia) opposite to it. This could be the medial compartment, or the lateral compartment.This can be seen on the left sided diagram on Image 1 below.
In a Total knee replacement (TKR) the entire distal (or furthest) portion of the femur, and the proximal (or nearest) portion of the tibia is replaced. Essentially, all three compartments of the knee joint are replaced. As mentioned above, this is also known as a total knee arthroplasty. An example of this is shown on the right sided diagram below.
TKR vs UKR
Generally, a UKR offers a shorter hospital stay and rehabilitation compared to a TKR (Pongcharoen et al; 2023). According to the Australian Orthopaedic Association (2015), 88% of knee replacement procedures are TKR’s, with UKR’s making up 5%, and revisions of previous procedures making up the remaining 7%.
| UKR | TKR | |
|---|---|---|
| DURABILITY | Roughly 10% have to be replaced in around 10 years | Roughly 5% have to be replaced in around 10 years |
| REHABILITATION | Rehabilitation usually only involves outpatient physio | Uncomplicated TKR's can rehab at home |
| RETURN TO FUNCTION | Around six weeks to return to most activities | 3 - 6 months to fully return to most activities |
| SATISFACTION | Around 90% of UKR patients would undergo the procedure again | Around 80% of TKR patients would undergo the procedure again |
| RISK OF COMMPLICATIONS | 3% experience complications in the first 12 months | 5% experience complications in the first 12 months |
Comparison of TKR Vs UKR (Informed Health, 2006)
Following the surgery
What will I experience initially?
Initially, individuals who undergo either a UKR or a TKR experience swelling, pain, and restricted knee range of motion. The main goal in hospital post surgery is to get you ready to return home in a safe manner as quickly as possible.
Swelling is usually quite severe initially, lasting for the first few weeks. Up to six months post surgery, mild to moderate swelling may persist. Swelling usually peaks in intensity 7-10 days post surgery.
Pain is often severe post total knee replacement. As a result, individuals are often prescribed strong painkillers (i.e. Endone) as a part of the initial management of symptoms.
Knee range of motion is usually addressed in a progressive nature with the input of a physiotherapist.
What comes next?
Post knee replacement, rehabilitation often commences on the same day. Typically TKR rehabilitation protocols occur for a longer duration, compared to a UKR. but the principles of rehabilitation are similar between both.
Weeks 0-3- Initial stages
This can involve a simple range of motion exercises in surrounding joints, and weight bearing (depending on surgeon's orders) on the affected side. Individuals who have undergone a UKR can commence more advanced resistance training.
Common Exercises: Ankle Pumps, Heel slides, Inner Range Quads, Passive knee straightening
Functional Training: Lying to Sitting, Sitting to Standing, Mobilising as tolerated (depending on surgeons orders)
Goals: Control pain, Improve swelling
Weeks 4-6- Intermediate stage
This stage involves progressive exercises compared to the previous stage. Individuals who have undergone a UKR can commence more advanced functional training earlier than TKR.
Common Exercises: Active range of motion, Heel raises
Functional Training: Normalising walking with a stick & progression to a single point stick
Goals: Knee flexion >90 degrees
Weeks 7 - 12- Advanced stage
This stage involves more functional progression, with an addition of resistance training & compound exercises (i.e. squats)
Common Exercises: Squats, Resisted knee range of motion (hamstrings, quads, adductors, gluteals)
Functional Training: Exercise bike, Supervised walking with a stick
Goals: Knee ROM 0 degrees extension - >110 degrees flexion
3+ Months- Maintenance
This stage is very patient specific. For more information on why, please read the section below.
Common Exercises: Exercise bike (increased distance), Return to gentle sports, Return to gentle gym workouts
Goals: Continue exercise program to optimise patient outcome from surgery
How long will it take to regain my function?
This is a complicated question, and it depends on your long term goals.
It is important to emphasise that a knee replacement will not allow you to engage in physical activity that you were unable to do prior to the surgery. Knee replacements are not designed to allow an individual to re-engage in high impact activities (AAHKS, 2017). The ability to engage in unlimited low impact activities, such as walking, golf, swimming, cycling etc. is a realistic goal.
Generally, it can take up to a year to recover fully from a total knee replacement, while it can take up to 4 months to recover fully from a unilateral knee replacement.
Wrap up
Knee pain contributes to a significant burden in Quality of life in many individuals. One of the chief contributing factors of knee pain is OA, particularly in individuals over the age of 45. Conservative management is typically the recommendation for people experiencing knee OA symptoms, with surgical interventions not indicated until conservative and symptomatic management fails to be enough. Physiotherapy led exercise programs like GLA:D have become increasingly popular due to the effectiveness of the intervention.
Rehabilitation post knee replacement generally consists of progressive range of motion, strengthening, and functional training. The duration of rehabilitation varies, depending on the nuanced presentation of your complaint and the type of surgery carried out. Whatever the case, an experienced physiotherapist will be able to work with you to help you regain your function again and maximise your outcomes following your surgery.